Bringing local outbreaks under control
Some recent examples show that outbreaks can be tackled although the mechanisms are still uncertain.
Welcome to Plugging the Gap (my email newsletter about Covid-19 and its economics). In case you don’t know me, I’m an economist and professor at the University of Toronto. I have written lots of books including, most recently, on Covid-19. You can follow me on twitter (@joshgans) or subscribe to this email newsletter here.
The past month has seen colleges reopened. Many have been online. Many have brought students back to campus or at least the local townships Universities may be in. There have been several media reports of outbreaks identifying the (mis)behaviour of college students who chose to party as soon as they saw each other again. If there was ever a more predictable behavioural outcome, I don’t know of it.
Alongside this has been a blame game. It was easy to blame the students but, in reality, their behaviour was not really different from many young people under Covid-19 and it was unclear how many students were really responsible. It was also easy to blame colleges for ‘opening up too early to save their own bacon.’ This is the sort of one-sided and simplistic motivation attribution that doesn’t work well. After all, if there is one thing a college administrator hates more than a budget deficit, it is a rash of bad publicity aimed squarely at them. They weren’t looking for that. More appropriately, it was a risk they chose to take.
The University of Illinois
Let’s look at one case that got a lot of early attention: the University of Illinois. This is a campus of some 40,000 students with an additional 6,000 staff that opened in August and immediately had a Covid-19 outbreak. This was of interest because they had done what we thought was the right thing: test everyone frequently. So what happened?
We know what happened. The students partied. That’s what the NYT reported. But testing should have covered that, right? The students can party if they have been tested and don’t have Covid-19. That’s the point of testing: to reduce the need for social distancing.
Did they not test? Well, the University has a terrific data dashboard that shows everything. They have done 400,000 tests since reopening which is about 15-20% of all tests done in the State! So they were covered there.
Did they not to appropriate modelling? Well, this xkcd cartoon suggested not:
The modelling team did have physicists but that wasn’t all. Moreover, the model did presume the students would party. What the model got wrong was that they also presumed that if a student tested positive, they would self-isolate and not go to parties. That turned out to be a bad assumption.
But notice what happened. Here is the data:

There was an outbreak about two weeks after the return to campus and then it was quickly dealt with via a 2-week lockdown. Put simply, the error in assumption was quickly picked up. The scale of the outbreak was known. And then it was dealt with and now there is a ‘normal’ flow of cases but no subsequent explosions. Of course, the semester is young but it tells us something.
It tells us that massive, scaled testing could work to bring about some normality. Here is an article that goes into the details of that scaled operation.
Once the university had a viable test, the team had to determine how often to use it, how to notify people of the results and then have a plan to isolate those who tested positive. "Fast and frequent" is the unofficial motto for the university's testing strategy.
"It really has to be that integrated, fast and frequent testing program to make the whole thing work," Burke said. "Because the pace at which the virus expands inside a person, you really do have a preciously short window of time to find out who's positive, quickly help them isolate safely and stop them from spreading it to others."
Initially, the school thought they'd test once a week, but based on modeling, realized that twice a week would be most effective.
At nearly 20 testing sites set up across campus, students and staff can walk up and self-administer a free COVID-19 test. They are advised to avoid eating, drinking, brushing their teeth, chewing gum or smoking an hour before submitting their sample. Swiping their school ID prints a barcoded sticker that goes on their testing tube. They dribble half a teaspoon of saliva into the tube and put it on a rack with other samples. The whole process takes about seven minutes, Burke said.
Every hour, the racks of samples are delivered by golf cart to the campus' veterinary lab and go straight into the hot water bath to deactivate the virus. The lab runs tests 24 hours a day on weekdays, and nearly that on weekends.
When the lab scans the barcode on the test tube, it connects to the person's medical record. The results of the test are delivered via a HIPAA-compliant secure portal or app, dubbed Safer Illinois, that UIUC created. App users can also opt in to a Bluetooth feature that alerts them if they've spent more than 15 minutes within 6 feet of a confirmed case and should get tested.
If faculty, staff and students receive a negative result at least every four days, they get a checkmark in the app and can enter campus buildings with their school ID. Some bars and restaurants are also using the app to let students gain entry, Burke said.
Another key feature of the school's COVID-19 strategy is isolating those who have tested positive as soon as possible. The university has found that the local health department has had trouble getting ahold of students promptly, with some students purposely ignoring the calls, Burke said, so it recently started directly reaching out to them. Its goal is to contact a positive case within 30 minutes and connect them with support.
They are now using what they have learned about this to expand testing beyond campus and into the local area.
San Quentin Prison
It is useful to compare this outcome to another place that had bad publicity. San Quentin state prison in California. This prison has some 3,000 inmates and in July had a large outbreak that left 26 people dead. The outcome is as tragic as it gets for this pandemic. But there was one silver lining. The outbreak ended.
Like the University of Illinois, the CA Corrections Department has provided a great data dashboard for all prisons in the state. Here is the data for San Quentin:
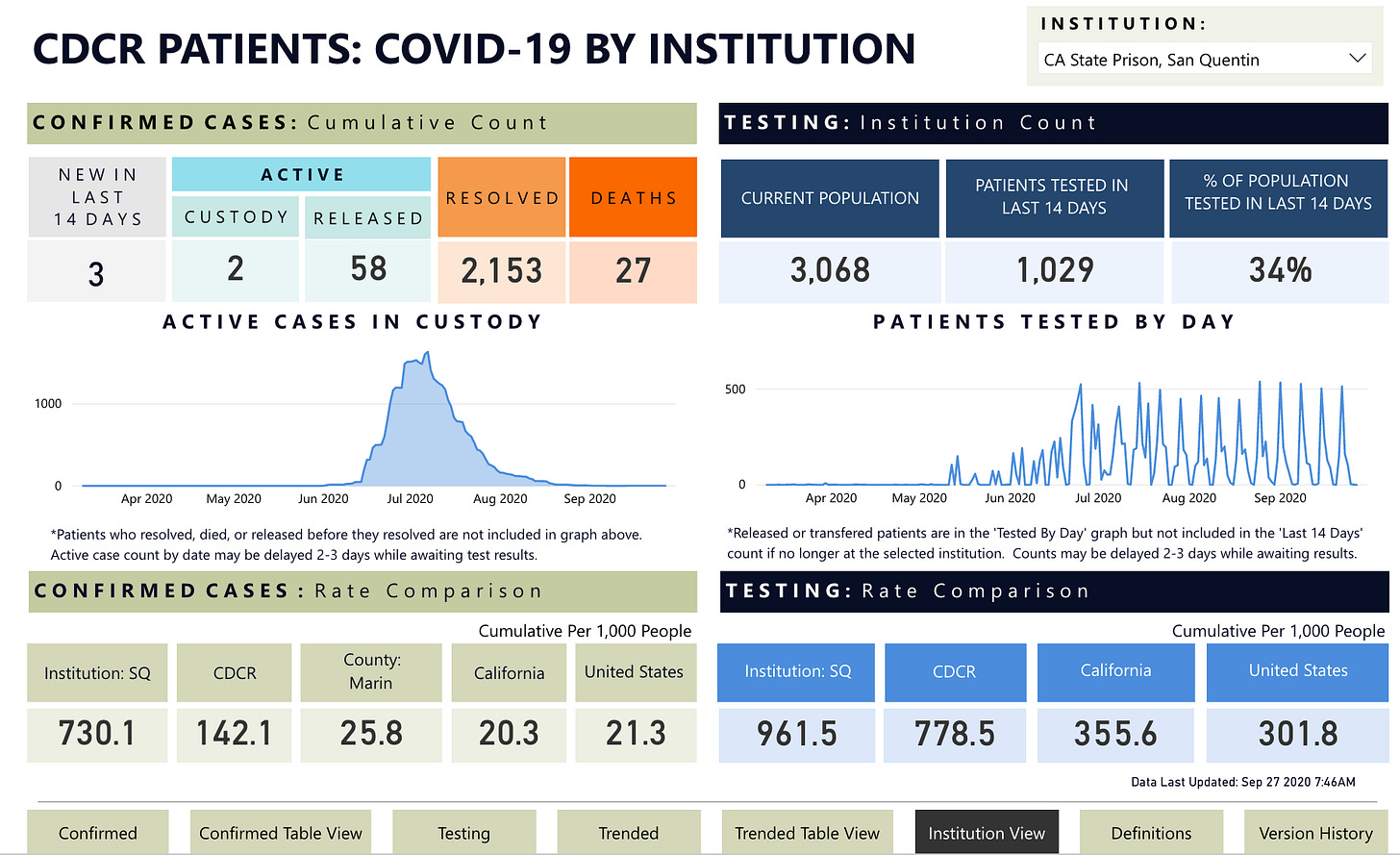
Notice that the outbreak ended. By that time two-thirds of the population had had Covid-19. Thus, it looks like herd immunity was reached at about 1/3 of the population which (a) tells us immunity is possible and (b) tells us what sort of outbreak we get if there is no real social distancing in place. On that score, the virus seemed to have run its course.
But we cannot be 100% sure. Why? Because look at the testing. It was really ramped up in July and every 2 weeks 1,000 inmates are tested. Just to calibrate, one suspects those the 1,000 inmates who are not yet immune to Covid-19 but it is hard to be sure. The testing coincides with the outbreak being brought under control. Thus, it may be testing that did it rather than immunity on its own.
The point, however, is that they have kept on testing and while there are some cases that emerge, they have not spread. In other words, in this literal bubble, testing appears to be forming a protective layer.
Summary
I provide both of these cases as food for thought. In each, there is widespread testing. in each, there are social distancing challenges. Does either give us a reason for optimism? I think so.
But there is another common factor: in both cases, there was a commitment to high data transparency. I tried, for instance, to look for data on Federal prisons in Texas that had big outbreaks but found nothing. My sense is that if we want widespread testing we should insist on data transparency so that we can all see what’s going on. That is the sort of disinfectant any of us can swallow.

