What does an infection tell us about others?
If someone tests positive for Covid-19, what does that tell us about where they got it?
Welcome to Plugging the Gap (my email newsletter about Covid-19 and its economics). In case you don’t know me, I’m an economist and professor at the University of Toronto. I have written lots of books including, most recently, on Covid-19. You can follow me on twitter (@joshgans) or subscribe to this email newsletter here.
If all goes well for the world, we may have screening protocols with rapid tests at many places by early next year. One thing that we should expect from that is that someone will test positive. Clearly, that person should not be cleared for entry and should be referred for proper testing and diagnosis. But what else should we do? In particular, what does that person testing positive tell us about whether others are likely to be infectious?
While there are some broad indicators that an infected person reveals, it turns out that precisely knowing what to do is not clear and involves some judgments regarding risk. I’ll try and explain this in today’s newsletter.
Broad Indicators
There is a temptation to treat a person who has Covid-19 as someone who may have spread it to others. So you ask that person who they had contact with over a certain period (let’s say a week). You are actually interested in who they had contact with and in what setting (e.g., outdoors or indoors) and for how long. Then you can identify people who should be tested. That way you get ahead of the viral spread.
The idea here is that if someone is positive for Covid-19, you want to assess when they were infectious and who they had contact with during that period. Of course, most tests don’t actually reveal that so it is a guess. If another test were taken and both had Ct scores listed you could probably trace likely contacts with more accuracy. (If you want to play at contact tracing yourself, I highly recommend this dashboard regarding a recent outbreak).
The goal here is to find contacts when the subject was infectious; so-called forward tracing. But there is another reason to trace contacts: to find out who infected the person in the first place. This is called backward tracing. In this case, what you want to find are contacts with the subject at the time they were likely to have become infected. Again, having the Ct score (with multiple time points) can assist in identifying the likely time range this might have happened. Otherwise, it is just a guess.
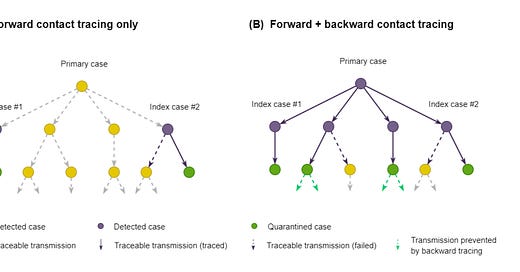
In principle, backward tracing can be more useful than forward tracing. A recent paper describes this and contains this useful illustration:

In this diagram, Index cases #1 and #2 have tested positive. Forward tracing would identify the green contacts. But backward tracing would hopefully find the primary case and their forward contacts. Mathematically, forward tracing identifies a subject’s R (reproduction number) while backward tracing as well gets you R scaled up by a factor related to the context of how an outbreak cluster arose.
Mathematically, this is all related to the Friendship Paradox which explains why your friends have more friends than you do. The reason is sampling bias. If you have a friend, then it is likely your friend has friends and because there are people out there who are really popular, the chances are that they are the one who are more popular than you. Statistically, you are not likely to be the popular one.
What if there is frequent testing?
Now suppose that you have a place, say, a school where you have frequent testing. (Obviously, we don’t have this, yet, but there are some places that do). Suppose that someone tests positive. You can then go and identify their forward contacts but the total number of people you would expect to pick up via that process is related to their R number. But if those people are having contact with others in that school, that R number will be quite low. In other words, the value of forward contact tracing is lower.
What about backward tracing? Here the value is enhanced. The likelihood is that the subject contracted the virus with a contact outside of the place. That means that there is value to others outside of the place to identify that contact. Thus, there is a strong case for backward tracing in this situation.
This means that if we evolve to a situation where we are screening people with tests for certain places, this will put a premium on backward tracing. In other words, if you want to invest in apps etc, that make tracing easier you want to ensure that your people use those apps outside of the place and hopefully encourage more people outside to have them. Keeping track of outside contacts is more important than keeping track of inside contacts.
This raises the obvious issue that there are externalities present in these decisions. Organisations will have a strong incentive to keep their places managed but a much lower incentive to do so for those outside which is precisely what backward tracing is designed to do. This is a pretty strong likely effect. I don’t have an easy answer for it but it does seem like it should be top of mind.
I should stress though that this is an effect and is not to detract from having rapid screens. Instead, it is to point out how doing so should potentially reorient our other efforts.
What did I miss?
Complacency