We need to plan for the worst
It is depressing to think about, but Covid-19 being endemic requires a different strategy
Welcome to Plugging the Gap (my email newsletter about Covid-19 and its economics). In case you don’t know me, I’m an economist and professor at the University of Toronto. I have written lots of books including, most recently, on Covid-19. You can follow me on Twitter (@joshgans) or subscribe to this email newsletter here.
Tim Harford had a hopeful article in the Financial Times a few weeks back considering how close we were to the light at the end of the tunnel. “Without minimising the suffering so many people are enduring, I think there is potential for rapid progress very soon. (I am writing these words at the end of January 2021.)” Now, as you read on with today's post, if you were looking for hope, the last sentence is all you are going to get. Warning: it is downhill from here.
Harford thought that it would take a little time but then vaccines would do their magic and before we knew it, the pandemic would be over. The article reflects the thinking of so many of us. I do it all of the time. I think of the pandemic as something that, like a war, can end. But this is really just a side-effect of The Ostrich Paradox (from a book by Robert Meyer and Howard Kunreuther) on why we are under-prepared for disasters. In the case of the pandemic, we are ignoring the most likely scenario: it never ends. That isn’t my opinion but the majority opinion of experts in the field.
I find the whole notion that the pandemic won’t ever end hard to cope with. When I wrote my first book on the subject, while I knew about this possibility, I disclaimed that I didn’t want to think about it and would take the view that a vaccine would eventually come. In the end, however, I grudgingly added the following, buried in the book:
What if it’s worse
Everything in this book thus far, as well as policy discussions regarding COVID-19, has been based on a very important assumption: once you have contracted the virus and recovered, you are immune. It is for this reason that epidemiologists focus on a sufficient share of the population obtaining immunity from COVID-19 either by past infection or as a result of a future vaccine. If you do this, then even with normal physical interactions, the virus eventually dies out (as R0 becomes less than 1). In particular, this is why we can talk about HAVE and HAD testing as making people safe again. So, while the crisis is awful, the promise of immunity gives us hope.
What if that hope is unfounded? What if you are not immune even if you have contracted the virus? What if a vaccine is not possible for the same reason? In this case, epidemiologists no longer use the SIR (susceptible–infected–removed) model, as there are no recovered people who are not able to infect others. Instead, we must use the SIS (susceptible–infected–susceptible) model. In that situation, when R0 exceeds one, the virus never goes away and a share of the population is always infected. The only way to get rid of the virus is by extreme measures—for instance, socially distancing until there are no more infected people or by coming up with treatments such that we don’t care if people are infected or not.
In many respects, some important parts of this fear have been allayed so much so that the book I published just last week(!) didn’t even entertain this possibility. The vaccines arrived and quickly and they are incredibly good. And if we are taking a scorecard approach, then on the immunity front there was good news too. But none of this has a scorecard. When it comes to immunity, the good is potentially the enemy of the perfect. A definitive end requires perfection and we don’t have perfection.
The endemic future
In 1918-20, we had a global pandemic that killed between 50 and 100 million people. How did that end? It didn’t. It became part of the seasonal flu cycle and we have it until this day. Indeed, given that it largely spared the elderly at the time, it is likely that it too was an offspring of past viruses that had been sporadically circulating. This happened in recent memory with H1N1 in 2009. There, older people were spared because they were likely infected back in a similar pandemic in the late 1960s.
Up until just the last couple of months, it looked like having had Covid-19 gave you immunity from reinfection. But in South Africa and Brazil recently, reinfection rates have been significant. Manaus had reached herd immunity and now was having a bigger outbreak. The cause is new variants. In the South African case, one vaccine trial has been halted because results were so poor. Although I should note that this was poor results regarding infection and not necessarily about contracting Covid-19, the disease, with severity. That distinction matters as I will explain shortly.
This was always the fear. The virus would mutate. Mutation is random but selection is not. Basically, expand the base upon which mutations can occur — that is, lots of people infected — and you empower selection. What is more, selection is potentially empowered when there is a challenge — such as existing immunity — because there is an opportunity for a variant that overcomes that immunity to ‘outperform’ mutations that don’t. Without existing immunity, the field is level-playing. And, moreover, it is one that has already jumped the big hurdle — human to human transmission. There is evidence the virus was circulating in bats 8 years ago (which, by the way, is the reason why the recent WHO finding that the virus likely originated from bats rather than the lab is bad news — if it was the lab, there wouldn’t be a reservoir of non-human potential sources of new coronaviruses). But it takes a leap to go from animals to humans and then between humans. SARS-CoV-2 has done that and so has the upper hand.
Therein lies the basic issue. If there was a world in which we suddenly jumped to full immunity, the mutation base would be eliminated and the evolutionary process crippled. But we don’t have that. We have widespread prevalence with some immunity and a slower vaccine rollout which tilts the playing field. In other words, this was the big cost of noting containing the virus as we did with SARS and MERS. It gets a foothold and we can’t shake it.
Planning for the worst
At the moment, we are still playing the ‘we can defeat Covid in a couple of years’ game. All economic planning, for instance, is done on that basis. In most wars, the participants are unduly optimistic about how quickly it will end; otherwise, we could probably avoid them. The pandemic is a war except that the enemy is not one we can psychologically break. But the question we have to ask ourselves now: is there a diplomatic solution? Is there a way to give the virus some of what it wants as a trade-off for something we want?
I know what you are thinking here: “he’s going to go all full, naturally acquired herd immunity on us, isn’t he.” No, I’m not. That isn’t a solution because we don’t want to get Covid-19 under the current conditions. The health consequences are too grave. Even with the elderly protected by vaccines, I think we have shown ourselves that the risks are too large and that we will still be actively trying to slow down that outcome.
But it is easy to start thinking that way. Here is The Economist on the subject:
For all these reasons, governments need to start planning for covid-19 as an endemic disease. Today they treat it as an emergency that will pass. To see how those ways of thinking differ, consider New Zealand, which has sought to be covid-free by bolting its doors against the world. In this way it has kept registered deaths down to just 25, but such a draconian policy makes no sense as a permanent defence: New Zealand is not North Korea. As vulnerable Kiwis are vaccinated, their country will come under growing pressure to open its borders—and hence to start to tolerate endemic covid-19 infections and deaths.
And I have to say that I do worry about the countries that have done well in the sense that they may have staved off the inevitable.
But the path to diplomacy is to think instead about treatments. There has been work on this but it hasn’t had the Operation Warp Speed mentality that we brought to vaccines. There are treatments now but let’s face it, the health consequences are still grave. The treatment we need are treatments that allow us to believe that this is more flu-like than plague-like. Indeed, the Astra Zeneca vaccine (whose trial was halted in South Africa) may actually be that. It may not prevent the virus from circulating but it may well prevent Covid-19, the disease. I don’t know, I’m not a medical doctor. But it is certainly not obvious to me that it isn’t a tool in a diplomatic solution with SARS-CoV-2 and its children.
Thusfar, we are holding up work on treatments. Many have raised concerns about this, especially with regard to repurposing existing treatments.
Analysis I have done with colleagues Susan Athey (economics of technology professor, Stanford Graduate School of Business), Richard Frank (professor of health economics, Harvard Medical School) and Jonathan Gruber (Ford professor of economics, MIT) suggests the repurposing of generic drugs that have already been proved safe and effective in treating other diseases is an important part of the solution, and there is an urgent need for government support. More than 100 generic drug candidates have been identified as having promise to treat the symptoms of Covid-19. Some are already being tested for their effectiveness. A focus on repurposing generic drugs would give researchers more shots on goal in the game of drug discovery, improving the odds that a winning treatment will emerge.
Suffice it to say, we are really behind here.
How will this play out
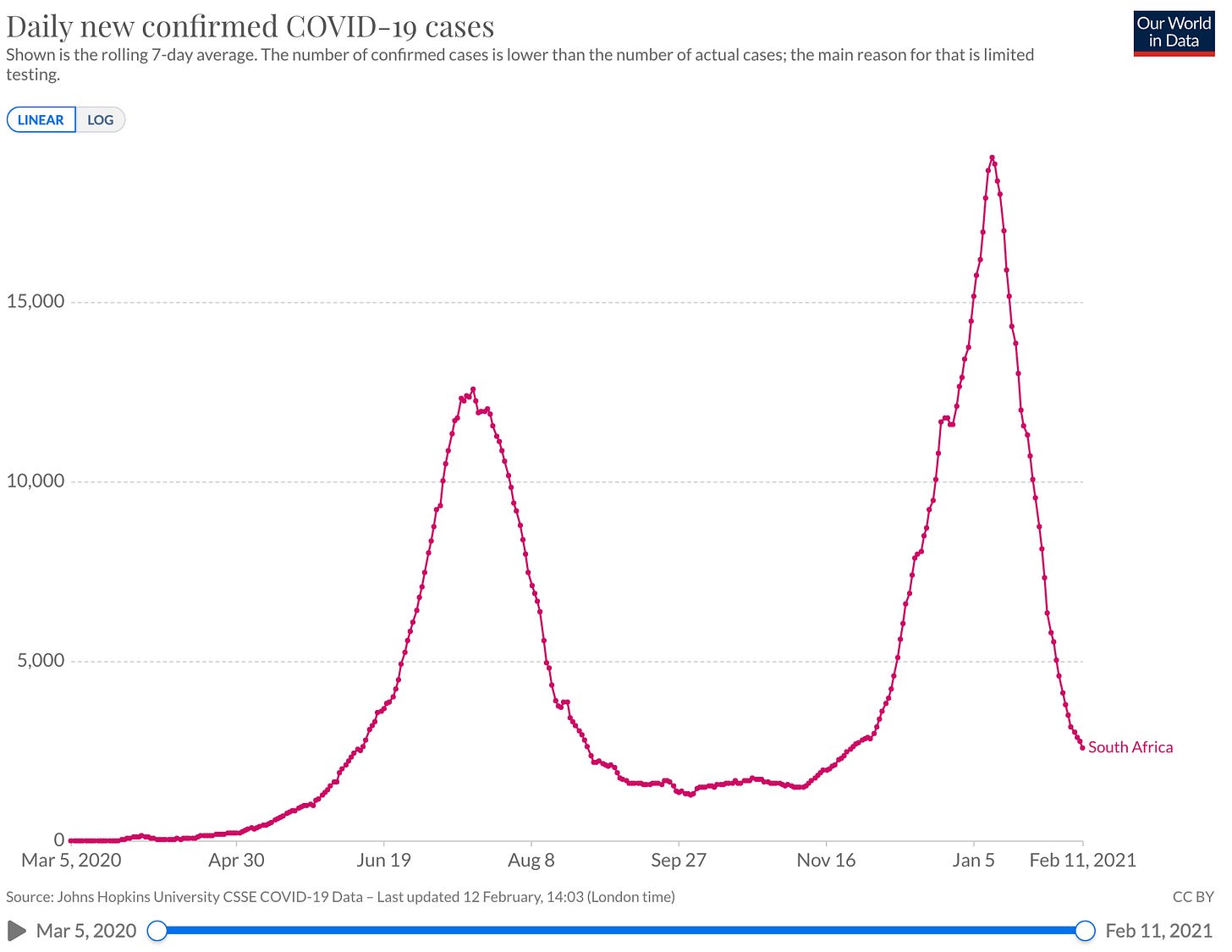
There is still plenty of uncertainty with regard to all of this. For instance, this is the current picture in South Africa. That is not a picture of a variant winning out.
That said, it may be a picture of summer heat winning out. Here is Michael Mina:
I think there’s a lot we don’t fully understand about immunity and the cycles of immunity and how strong our immune systems are during the winter. It’s a huge thing. How many kids get really bad colds and come home all snotty during the summer? The winter — it’s a real thing! But we don’t fully understand why. And vitamin D and sunlight could certainly play a role. Generally scientists and biologists and even physicians oddly throw the most natural explanations under the bus, and say no way. But we are evolved creatures — we evolved on Earth without roofs over our head. It’s insane to think that something like sunlight would not affect us in some way. And we know people get seasonal depressive disorder because of a lack of sunlight, so very clearly it has major impacts on us, and to discount it just because it’s sunlight and not some molecule that …
You can sell.
Yeah, exactly. I’m always astounded at how many physicians just immediately discount all this stuff. We know that vitamin D has a huge interaction with immunity, that’s not even in question. And so I definitely think that could very well be part of it. Is it the primary source of variance or is it just a piece of the puzzle? I would probably say it’s likely a piece of the puzzle.
This is, of course, the reason why epidemiologists expect the largest outbreaks in Europe and North America will be in March-April. We are going to relax restrictions in February-March and then it will come surging back. The summer will then see a decline in cases but it represents an opportunity to break the back of Covid-19 and speed the transition to something manageable. We need to have vaccinated all adults by September. There are risks to the kids but those are risks that we have to learn to manage going forward as there are going to be more kids.
The Atlantic spells out what this means after this point:
What does that mean for the future of COVID-19? One possible scenario is that the disease could follow the path of the four coronaviruses that cause common colds, which frequently reinfect people but rarely seriously. In one study that tried to infect and then reinfect volunteers with one of these common-cold coronaviruses one year apart, some of the volunteers indeed got reinfected but without symptoms. They also had detectable amounts of the virus in their nose for a shorter period of time. For COVID-19, “the optimistic future is that there are still infections but they are less frequent than now,” Jesse Bloom, a virologist at the Fred Hutchinson Cancer Research Center, wrote in an email, “and most infected people have something more resembling a cold than a life-threatening infection.” (There is speculation, in fact, that the coronavirus OC43 emerged during an 1889 pandemic before fading into the background as a common cold.)
Lavine, at Emory, has co-authored a paper modeling how COVID-19 could eventually end up like these cold coronaviruses. The four that already exist are so common that most of us were probably infected with them in childhood. This early encounter lays down initial immunity against these coronaviruses so that reinfections later in life are milder. Frequent reinfection, when immunity fades and the cold coronavirus evolves, may also update that immunity.
COVID-19 is clearly and dramatically more deadly for older patients. We might think of the vaccines, then, as a replacement for the immunity that adults never got to build against COVID-19 as children. But because this is a new coronavirus, Lavine cautions about uncertainties that remain, especially in how new variants may continue to evolve and whether immunity first elicited in adulthood is equivalent to immunity first elicited in childhood.
In other words, we continue the war through the summer and then move to the diplomatic solution just like we did with coronaviruses of old. But at the same time, a diplomatic solution needs institutional backing. In our case, we need our information solution to be on-going and able to ramp up and down as the case may be. Here is Mina again:
What’s else do you have in mind?
I’ve been trying for years to start a global immunological observatory to prevent outbreaks just like this. And for years I’ve been told, “This is too expensive. This is too costly. Why would we ever do this? We’ll deal with it when the disease comes around.” Well, you know, now it’s come around and we didn’t have any global surveillance set up for novel outbreaks. But imagine we had started five years ago to build a weather system for viruses. We could’ve potentially prevented this year from happening.How would you get all that data?
There’s a few things that are constant across the whole globe. Two of them are, when people get sick they get blood tests, and people donate blood, Blood samples taken in pretty much every single town and city in the world. But the moment that the result the doctors wanted to get is done, they throw away the tubes of blood. Well, what if those tubes weren’t thrown away? What if they were all packaged up and sent to a government facility or franchised immunological observatory labs, and processed with a core set of immunological tools that would give you an understanding of all the pathogens people see. And it can all be de-identified, so it wouldn’t be traced back to individuals. It would turn us all into little weather buoys for infectious disease.And if we can compile those samples, we could then take all these new technologies where we can take a drop of blood, just literally less than a drop, and I could tell you all of the pathogens that you have ever seen in your life.
No light
It is time to start understanding this whole issue. It is complex precisely because our vaccine strategy — being as it is a tool of war rather than diplomacy — can impact on our ability to manage an endemic disease as this recent paper highlights. We don’t have all of the answers here. What I know is that someone needs to be on the case and we likely need to start preparing our policy-makers and population for this possibility. It has huge impacts on economic forecasts. I’ll likely have more to say about this issue in future posts. With our heads in the sand, the experts have just not written enough about this outcome. It is time for everyone to pull them out and get serious.